Costantini Lara, et al.
International journal of molecular sciences, 2017
Abstract
Long-term dietary habits play a crucial role in creating a host-specific gut microbiota community in humans. Despite the many publications about the effects of carbohydrates (prebiotic fibers), the impact of dietary fats, such as omega-3 polyunsaturated fatty acids (PUFAs), on the gut microbiota is less well defined. The few studies completed in adults showed some common changes in the gut microbiota after omega-3 PUFA supplementation. In particular, a decrease in Faecalibacterium, often associated with an increase in the Bacteroidetes and butyrate-producing bacteria belonging to the Lachnospiraceae family, has been observed. Coincidentally, a dysbiosis of these taxa is found in patients with inflammatory bowel disease. Omega-3 PUFAs can exert a positive action by reverting the microbiota composition in these diseases, and increase the production of anti-inflammatory compounds, like short-chain fatty acids. In addition, accumulating evidence in animal model studies indicates that the interplay between gut microbiota, omega-3 fatty acids, and immunity helps to maintain the intestinal wall integrity and interacts with host immune cells. Finally, human and animal studies have highlighted the ability of omega-3 PUFAs to influence the gut-brain axis, acting through gut microbiota composition. From these findings, the importance of the omega-3 connection to the microbiota emerges, encouraging further studies.
Keywords
DHA; EPA; behavioral disorders; dysbiosis; gut microbiota; inflammation; omega-3 PUFAs.
Conflict of interest statement
The authors declare no conflict of interest.Figures
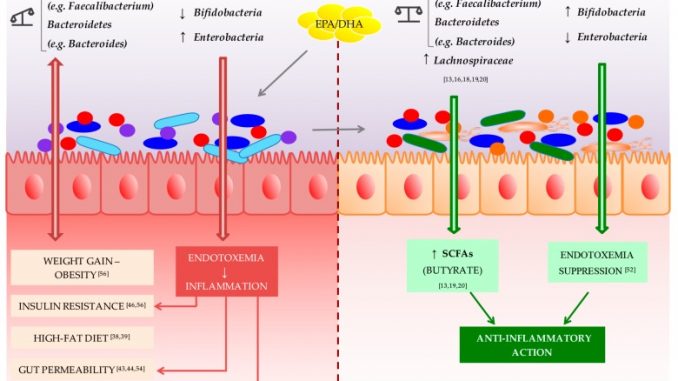
Omega-3 polyunsaturated fatty acid (PUFA) potential action in restoring eubiosis in gut microbiota. Dysbiosis of the Firmicutes/Bacteroidetes ratio is associated with several conditions, such as weight gain and obesity [56], insulin resistance [56], high-fat diet [38,39], gut permeability [54], IBDs [21], and depression [88]. Similarly, a Bifidobacteria decrease combined with a Enterobacteria increase leads to the establishment of endotoxemia that causes a chronic low-grade inflammation associated with some pathological conditions, like insulin resistance [46], gut permeability [43,44], and depression [92]. Initial evidence shows that omega-3 PUFAs are able to reverse this condition by restoring the Firmicutes/Bacteroidetes ratio, and increasing Lachnospiraceae taxa [13,16,18,19,20], both associated with an increased production of the anti-inflammatory short-chain fatty acid (SCFA) butyrate [13,19,20]. Moreover, animal studies showed the ability of omega-3 PUFAs to increase lipopolysaccharide (LPS)-suppressing bacteria, Bifidobacteria, and to decrease LPS-producing bacteria, Enterobacteria, negating the endotoxemia phenomenon [52]. For all these actions, omega-3 PUFAs can be considered as prebiotics, able to restore gut eubiosis in some pathological conditions.
| PMID: | 29215589 |
|---|---|
| DOI: | 10.3390/ijms18122645 |
| PMCID (Free PMC Article): | PMC5751248 |
| Category: | Digestive Health |
Previous article
Effects of Omega-3 Fatty Acids on Immune Cells.
Next article
Marine omega-3 Fatty Acids and Inflammatory Processes: Effects, Mechanisms and Clinical Relevance.

























































