Carlberg Carsten, et al.
Nutrients, 2019
Abstract
Nutrigenomics studies how environmental factors, such as food intake and lifestyle, influence the expression of the genome. Vitamin D₃ represents a master example of nutrigenomics, since via its metabolite 1α,25-dihydroxyvitamin D₃, which binds with high-affinity to the vitamin D receptor, the secosteroid directly affects the epigenome and transcriptome at thousands of loci within the human genome. Vitamin D is important for both cellular metabolism and immunity, as it controls calcium homeostasis and modulates the response of the innate and adaptive immune system. At sufficient UV-B exposure, humans can synthesize vitamin D₃ endogenously in their skin, but today's lifestyle often makes the molecule a true vitamin and micronutrient that needs to be taken up by diet or supplementation with pills. The individual's molecular response to vitamin D requires personalized supplementation with vitamin D₃, in order to obtain optimized clinical benefits in the prevention of osteoporosis, sarcopenia, autoimmune diseases, and possibly different types of cancer. The importance of endogenous synthesis of vitamin D₃ created an evolutionary pressure for reduced skin pigmentation, when, during the past 50,000 years, modern humans migrated from Africa towards Asia and Europe. This review will discuss different aspects of how vitamin D interacts with the human genome, focusing on nutritional epigenomics in context of immune responses. This should lead to a better understanding of the clinical benefits of vitamin D.
Keywords
VDR; Vitamin D; evolution; immune system; nutritional epigenomics; transcriptome.
Conflict of interest statement
The author declares no conflict of interest.Figures
 Vitamin D3 is synthesized endogenously in UV-B exposed human skin" width="739" height="924" class="size-full wp-image-3836" />
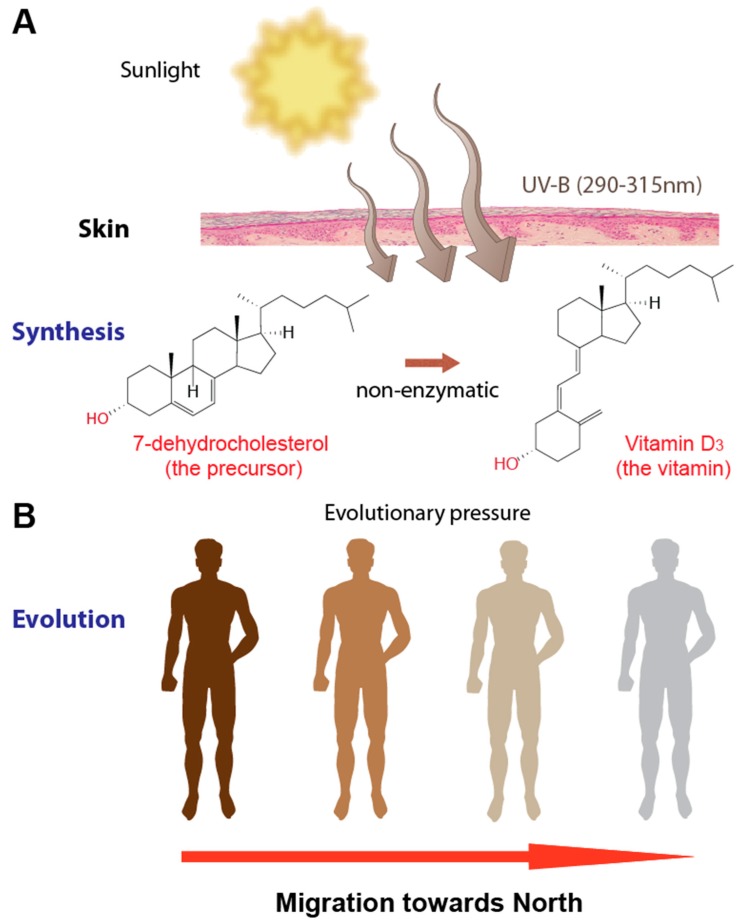
Vitamin D3 is synthesized endogenously in UV-B exposed human skin" width="739" height="924" class="size-full wp-image-3836" />Vitamin D and human skin. Vitamin D3 is synthesized endogenously in UV-B exposed human skin (A). During the past 10–30,000 years this essential need to synthesize vitamin D3 was an evolutionary driver for skin lightening of modern humans migrating from Africa towards Europe and Asia (B).
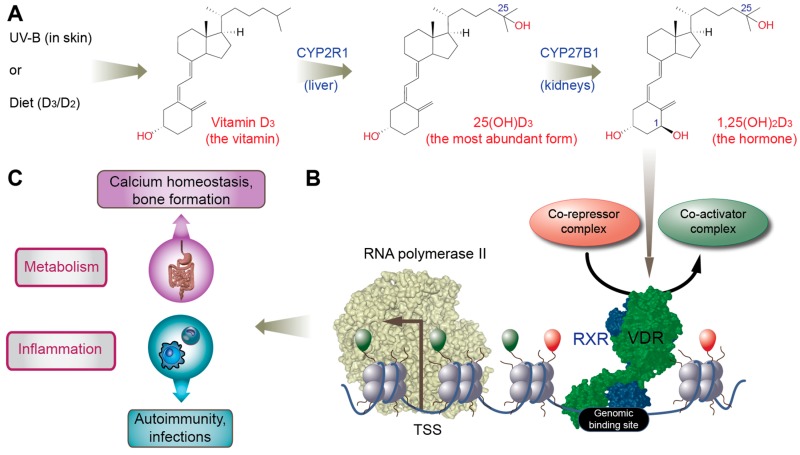
Gene regulation by vitamin D and its physiological impact. Vitamin D3, produced endogenously in skin or taken up by diet or supplementation, is converted in the liver into 25(OH)D3 and then in the kidneys into the high-affinity vitamin D receptor (VDR) ligand 1,25(OH)2D3 (A). Ligand-activated VDR binds genome-wide to some 5–20,000 sites within accessible chromatin (B). Some of these epigenome-wide effects translate into the changes of the transcriptome, i.e., the activation (or repression) of vitamin D target genes. The main physiological processes regulated by these genes are cellular metabolism, such as calcium homeostasis important for bone formation, and the regulation of innate and adaptive immunity, such as improving the response to infectious microbes, reducing chronic inflammation and preventing autoimmune disease (C).
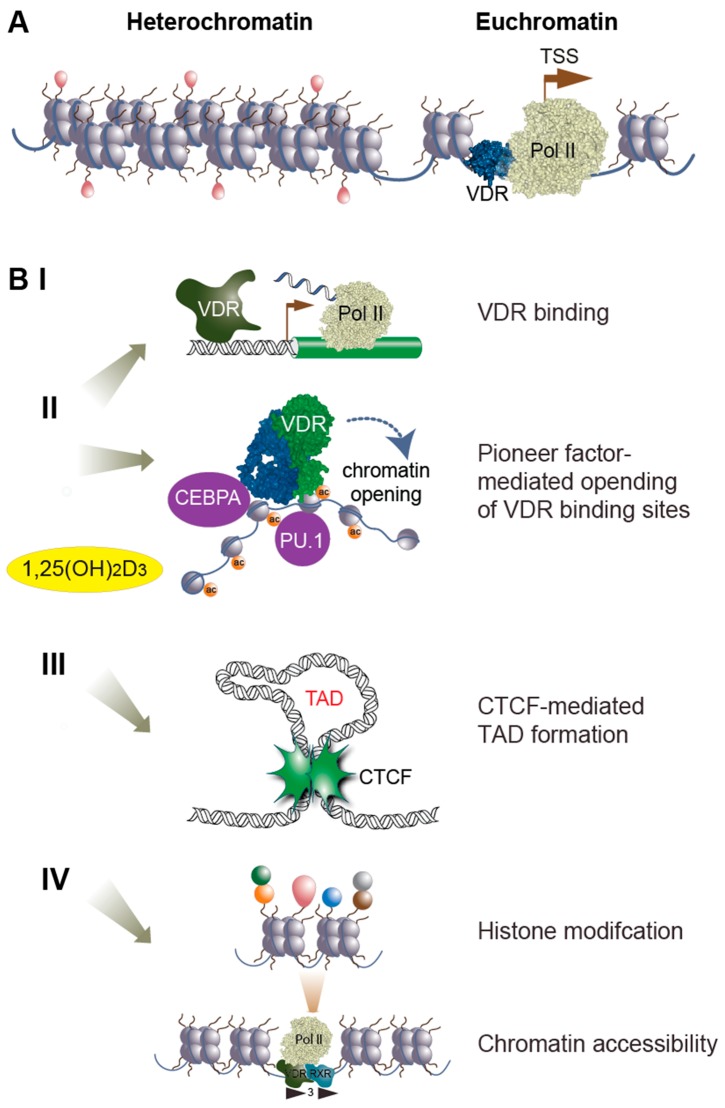
Vitamin D and the epigenome. Chromatin is segregated into non-accessible heterochromatin and euchromatin, where VDR can find its genomic binding sites (A). Vitamin D can influence the epigenome in multiple ways (B), such as increasing genomic VDR binding (I), affecting the binding of pioneer transcription factor (II), influencing CCCTC binding factor (CTCF) binding and the formation of topologically associated domains (TADs) (III) and changing histone modifications and chromatin accessibility (IV)
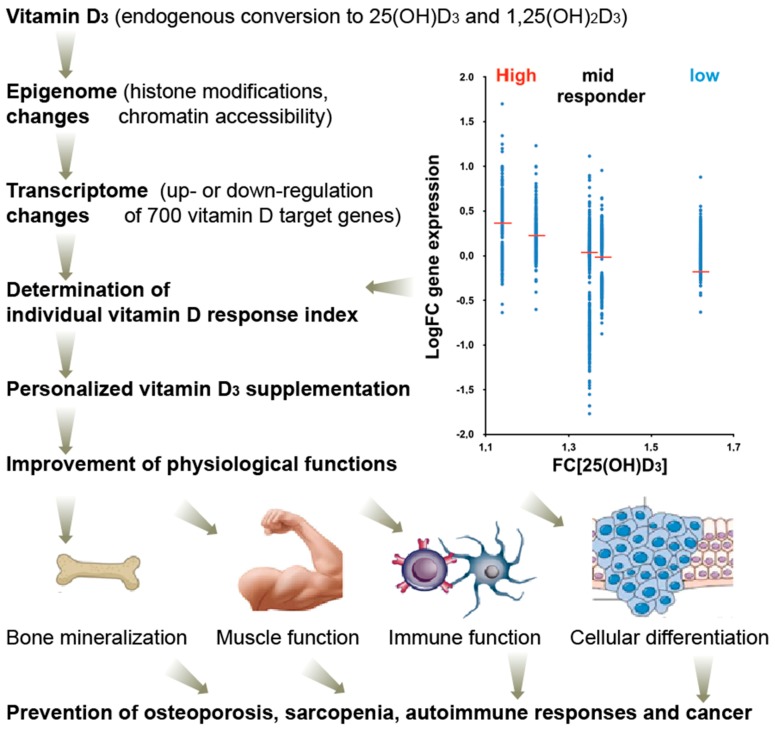
Clinical benefits of optimized vitamin D action. The vitamin D response index segregates individuals into high, mid, and low vitamin D responders and allows a more accurate monitoring of vitamin D effects in clinical setups, such as a prevention of osteoporosis, sarcopenia, autoimmune diseases, and possibly even cancer. The index is based on individual’s genetic and epigenetic status, but does not depend on their vitamin D status. It is determined primarily via changes of the transcriptome (i.e., mRNA transcription of vitamin D target genes) of vitamin D responding tissues, such as PBMCs. FC, fold change.
| PMID: | 30901909 |
|---|---|
| DOI: | PMC6470874 |
| PMCID (Free PMC Article): | 10.3390/nu11030676 |
| Category: | Allergy / Immune |
The best supplements with Cholecalciferol in Allergy / Immune category:
- D3, 25 mcg (1,000 IU), 110 Tablets (21st Century) - Vitamin D3 is essential for absorption of calcium and support bone, teeth, and immune system health. It contains among others: Cholecalciferol.
- Vitamin D3 (Cholecalciferol), 25 mcg (1,000 IU), 250 Softgels (Solgar) - Vitamin D is a fat-soluble vitamin that is required to promote calcium absorption, which helps to maintain healthy bones and teeth. It contains among others: Cholecalciferol.
- Vitamin D3 (Cholecalciferol), 125 mcg (5,000 IU), 100 Softgels (Solgar) - Vitamin D is required to promote calcium absorption, which helps to maintain healthy bones and teeth. It contains among others: Cholecalciferol.
- Vitamin D3 (Cholecalciferol), 250 mcg (10,000 IU), 120 Softgels (Solgar) - Vitamin D is required to promote calcium absorption, which helps to maintain healthy bones and teeth. It contains among others: Cholecalciferol.
- Vitamin D-3, High Potency, 2,000 IU, 30 Softgels (Now Foods) - NOW Vitamin D-3 softgels supply this key vitamin in a highly absorbable liquid softgel form. It contains among others: Cholecalciferol.
- Vitamin D-3, High Potency, 5,000 IU, 240 Softgels (Now Foods) - NOW Vitamin D-3 softgels supply this key vitamin in a highly-absorbable liquid softgel form. It contains among others: Cholecalciferol.
- Vitamin D-3 High Potency, 10,000 IU, 120 Softgels (Now Foods) - NOW Vitamin D-3 softgels supply this key vitamin in a highly-absorbable liquid softgel form. It contains among others: Cholecalciferol.
- Vitamin D-3, High Potency, 5,000 IU, 120 Softgels (Now Foods) - NOW Vitamin D-3 softgels supply this key vitamin in a highly-absorbable liquid softgel form. It contains among others: Cholecalciferol.
Articles similar to "Nutrigenomics of Vitamin D."
- The significance of Cholecalciferol for Allergy / Immune: Regulation of Immune Function by Vitamin D and Its Use in Diseases of Immunity. (Evidence exists for a role for vitamin D and its active metabolites in modulating immune functions...)
- The impact of Cholecalciferol on Allergy / Immune: Vitamin D Supplementation During Pregnancy: Effect on the Neonatal Immune System in a Randomized Controlled Trial. ( Programming of the immune system during fetal development can influence asthma-related risk factors and outcomes in later life... Vitamin D exposure during fetal development influences the immune system of the neonate, which can contribute to protection from asthma-related, including infectious, outcomes in early life. Trial registration: ClinicalTrials.gov NCT00920621. )
- The significance of Cholecalciferol for Allergy / Immune: The Active Metabolite of Vitamin D3 as a Potential Immunomodulator. (In the past, vitamin D was known for its classical, skeletal action as a regulator of calcium and bone homoeostasis... Vitamin D exposure during fetal development influences the immune system of the neonate, which can contribute to protection from asthma-related, including infectious, outcomes in early life. Trial registration: ClinicalTrials.gov NCT00920621. )
- The role of Cholecalciferol in Allergy / Immune: Vitamin D Treatment Modulates Immune Activation in Cystic Fibrosis. (Persistent inflammatory response in cystic fibrosis (CF) airways is believed to play a central role in the progression of lung damage... Vitamin D exposure during fetal development influences the immune system of the neonate, which can contribute to protection from asthma-related, including infectious, outcomes in early life. Trial registration: ClinicalTrials.gov NCT00920621. )
Previous article
Vitamin D Treatment Modulates Immune Activation in Cystic Fibrosis.

























































